Fungal Infections: A Growing Threat Of Antibiotic Resistance
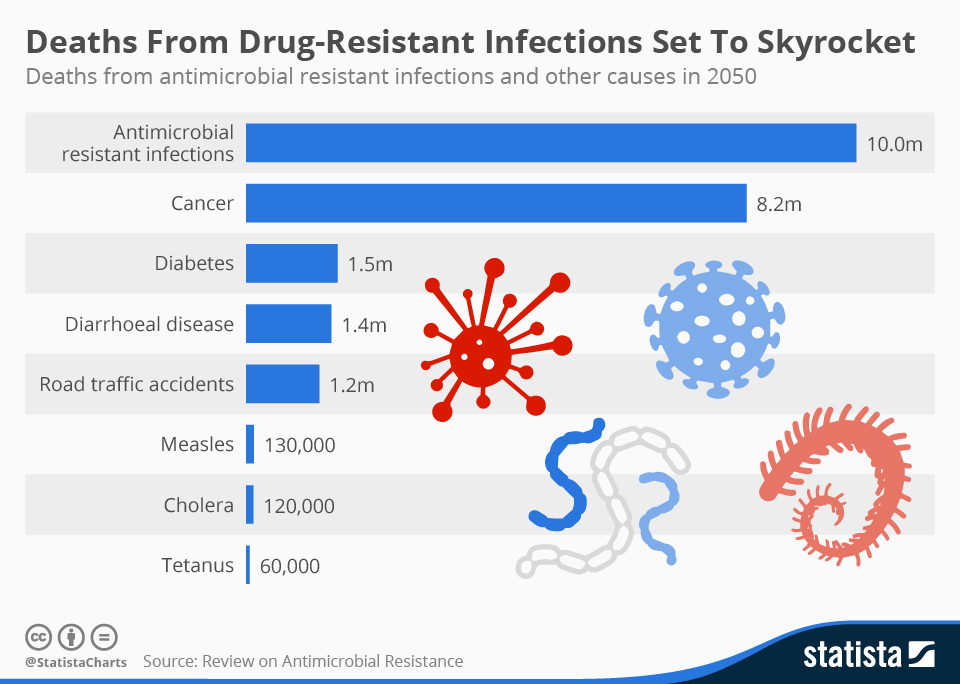
Table of Contents
The Rise of Antifungal Resistance
The development of antifungal resistance is a complex process, significantly hampered by the limited number of antifungal drugs available. Understanding the mechanisms of antifungal resistance is paramount to developing effective countermeasures.
Mechanisms of Antifungal Resistance
Fungi employ various strategies to evade the effects of antifungal drugs. These antifungal resistance mechanisms include:
-
Target modification: Fungi can alter the target site of the antifungal drug, rendering it ineffective. This is common with azoles, which target ergosterol biosynthesis. Mutations in genes encoding enzymes involved in this pathway can lead to azole resistance.
-
Efflux pumps: Many fungi possess efflux pumps that actively expel antifungal drugs from the cell, reducing their intracellular concentration. This mechanism contributes to resistance against various classes of antifungals.
-
Altered drug metabolism: Fungi can modify the structure of the antifungal drug, making it less effective or inactive. This is particularly relevant to some echinocandins.
-
Specific examples of resistant fungal species: The emergence of Candida auris, a highly resistant species, has caused significant alarm globally. Similarly, Aspergillus fumigatus, a common cause of invasive aspergillosis, is increasingly exhibiting resistance to azoles and echinocandins. Understanding the echinocandin resistance mechanisms in these species is crucial for developing new treatment strategies.
-
Overuse and misuse of antifungals: The widespread use of antifungals in both human and veterinary medicine, as well as in agriculture, has significantly contributed to the selection and spread of resistant strains. Inappropriate use and broad-spectrum antifungal prescriptions accelerate this process.
-
Impact of agricultural antifungal use: The application of antifungals in agriculture contributes significantly to the development and spread of resistant fungi. These resistant strains can then spread to humans and animals through the food chain or the environment.
Impact of Fungal Infections on Human Health
Fungal infections affect a broad spectrum of individuals, but certain populations are particularly vulnerable to severe infections. The impact of these infections on human health is substantial and far-reaching.
Vulnerable Populations
Several groups are at significantly higher risk of developing serious fungal infections, including:
-
Immunocompromised patients: Individuals with weakened immune systems, such as those with HIV/AIDS, cancer, or undergoing organ transplantation, are highly susceptible to opportunistic fungal infections. These infections can be life-threatening.
-
Patients with chronic illnesses: Individuals with chronic conditions like diabetes, cystic fibrosis, and chronic obstructive pulmonary disease (COPD) are also at increased risk.
-
Hospitalized patients: Healthcare settings are often reservoirs for resistant fungal pathogens, leading to increased risk of nosocomial fungal infections.
-
Severity and mortality rates: Invasive fungal infections have high mortality rates, often exceeding 50% in certain cases. Early diagnosis and appropriate treatment are critical to improving outcomes.
-
Impact on healthcare systems: The rise of antifungal-resistant infections has a considerable impact on healthcare systems, leading to increased hospitalization durations, higher treatment costs, and a greater burden on healthcare resources.
-
Potential for spread in healthcare settings: The spread of resistant fungal pathogens in healthcare facilities poses a considerable risk, particularly to vulnerable patients. Implementing rigorous infection control measures is crucial to mitigate this risk.
Diagnosis and Treatment of Fungal Infections
Diagnosing and treating fungal infections effectively presents significant challenges, particularly in the context of growing antifungal resistance.
Challenges in Diagnosis
Early and accurate diagnosis is critical for effective treatment and improved patient outcomes. However, diagnosing fungal infections can be difficult due to several factors:
-
Time-consuming culture and identification: Traditional methods of fungal diagnosis, such as culture and microscopic examination, can be time-consuming, potentially delaying appropriate treatment. This delay is particularly crucial in severe infections. The need for rapid diagnostic tests for fungal infections is therefore paramount.
-
Use of various diagnostic techniques: A range of diagnostic techniques are employed, including microscopy, culture, and molecular tests (PCR). The choice of method depends on the suspected infection and the resources available. The development and implementation of better molecular diagnostics are crucial.
-
Importance of early and accurate diagnosis: Early diagnosis is crucial to prevent progression to severe disease and to guide appropriate antifungal therapy.
Current and Future Treatment Strategies
Existing antifungal drugs, while effective against some fungal species, have limitations, especially concerning resistance. Research into new therapies is crucial.
-
Existing antifungal drugs and their limitations: The limited number of antifungal drug classes and the emergence of resistance necessitate a search for novel therapeutic agents.
-
Use of combination therapy to overcome resistance: Combining different classes of antifungal drugs can help overcome resistance mechanisms, preventing the development of further resistance.
-
Role of stewardship programs in combating antifungal resistance: Implementing antifungal stewardship programs aims to optimize antifungal use, minimize resistance development, and improve patient outcomes.
-
Ongoing research in novel antifungal therapies: Research is actively pursuing novel antifungal therapies, including immunotherapies and new drug classes targeting different fungal pathways. This includes research into new antifungal drugs and improved antifungal drug development strategies.
Conclusion
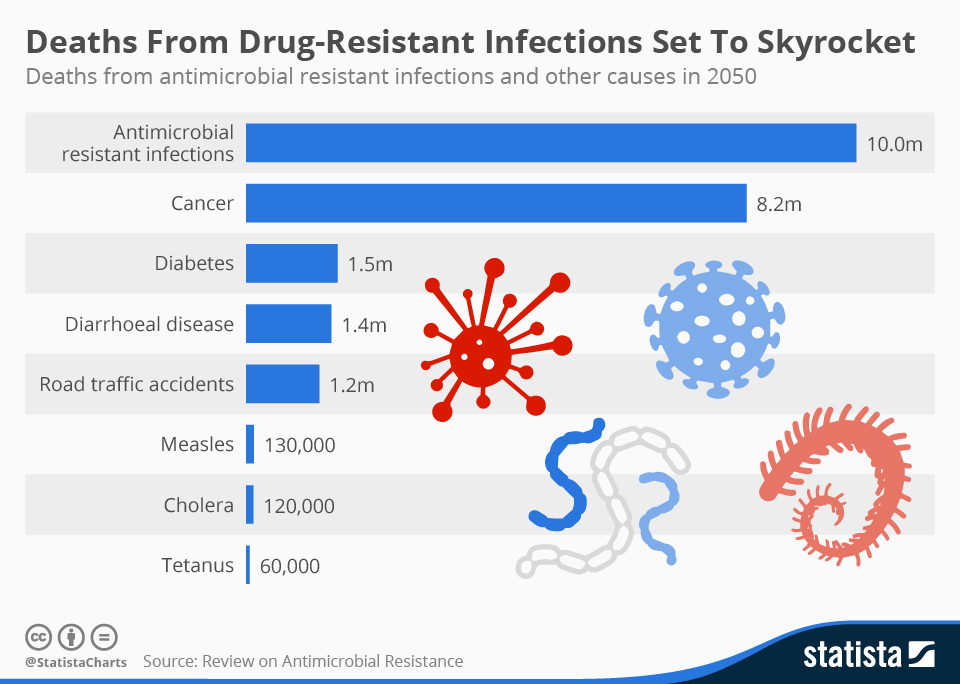
The escalating threat of fungal infections, exacerbated by the rise of antifungal resistance, presents a major challenge to global public health. The impact on vulnerable populations, healthcare systems, and the overall disease burden is substantial. Challenges in diagnosis and limitations of current treatments highlight the urgent need for innovative solutions. We must prioritize research into new antifungal drugs, improved diagnostic tools, and effective infection control strategies. Increased awareness, improved antifungal stewardship, and robust funding for research are essential in combating this growing threat. Learn more about protecting yourself from fungal infections and support research into new antifungal therapies to help curb this growing global health issue. Advocate for improved infection control practices to combat the growing threat of fungal infections and help save lives.
Featured Posts
-
 New In Kenya Uber One Membership With Exclusive Discounts And Free Deliveries
May 08, 2025
New In Kenya Uber One Membership With Exclusive Discounts And Free Deliveries
May 08, 2025 -
 Xrps Strong Performance Surpassing Bitcoin And Other Cryptocurrencies After Sec Action
May 08, 2025
Xrps Strong Performance Surpassing Bitcoin And Other Cryptocurrencies After Sec Action
May 08, 2025 -
 Ethereums Bullish Run Price Analysis And Future Predictions
May 08, 2025
Ethereums Bullish Run Price Analysis And Future Predictions
May 08, 2025 -
 Trade War Fallout Which Cryptocurrency Will Prevail
May 08, 2025
Trade War Fallout Which Cryptocurrency Will Prevail
May 08, 2025 -
 Ekonomi Haberleri Bakan Simsek Ten Kripto Para Piyasasina Yeni Uyarilar
May 08, 2025
Ekonomi Haberleri Bakan Simsek Ten Kripto Para Piyasasina Yeni Uyarilar
May 08, 2025
